If you are over 65, please visit vaccines.nh.gov to sign up today for your COVID-19 vaccine or you can call 211. If you are our patient, are under age 65 and have two or more chronic conditions, please call (603) 527-7069 for assistance.
When can I get a COVID-19 Vaccine in New Hampshire?
Phase 1B is the next group of New Hampshire residents to be vaccinated. This is specific for:
- People 65 years and older, OR;
- Those under the age of 65 and have 2 or more high-risk health conditions.
Those conditions are defined as:
- Cancer
- Chronic Kidney Disease
- COPD or high-risk pulmonary disease
- Down Syndrome
- Heart condition (heart failure, coronary artery disease, cardiomyopathy)
- Immunocompromised states
- Obesity (BMI >30kg/m)
- Pregnancy
- Sickle Cell Disease
- Type 2 Diabetes
Our priority is to get you vaccinated as quickly as possible.
Vaccination plans are evolving quickly and we are actively working with the State of New Hampshire to understand the distribution plans.
NOTE: WE ARE WAITING FOR CONFIRMATION OF EXACTLY HOW MANY VACCINES WE WILL RECEIVE AND WHEN THEY ARE ARRIVING. CONTINTUE TO MONITOR https://concordhospital-laconia.org/coronavirus FOR FURTHER INFORMATION
COVID-19 RESOURCES
Who can receive a vaccination at LRGHeatlhcare?
LRGHealthcare is considered an open site. That means that any New Hampshire resident who satisfies eligibility can receive the vaccine at either Franklin Regional Hospital or Lakes Region Hospital. Dates, days and times will be posted on the COVID-19 Vaccine Administration Management System (VAMS) site through the CDC and is dependent on supply of vaccines.
PLEASE NOTE: ONLY THOSE WHO HAVE A CONFIRMED APPOINTMENT THROUGH COVID-19 Vaccine Administration Management System (VAMS) site through the CDC WILL RECEIVED THE VACCINE.
- If you are an LRGH patient and meet the criteria of 65 or younger and have 2 chronic health conditions please call THE LRGH CALL CENTER AT 603-527-7069.
ALL others please go to vaccines.nh.gov or call 2-1-1.
What should you do next?
- If you are a LRGHealthcare patient who is 64 years of age or younger, and have 2 or more high risk health conditions: (refer to list above)
- Please call the COVID-19 Hotline at 603-527-7069, Monday through Friday, 8am to 4pm or email to: covidvaccine@lrgh.org
- You will be sent an email to sign up for your vaccine. This is through the COVID-19 Vaccine Administration Management System (VAMS) site through the CDC. Please see this PDF for instructions on using the site.
- If you are a New Hampshire resident 65 years of age or older: Visit the State website beginning at 8:00am on Friday, January 22, 2021 to schedule your vaccination. https://www.vaccines.nh.gov
- If you are a New Hampshire resident, 65 years of age and younger with 2 or more high risk health conditions, (refer to list above) and NOT an LRGH patient: Visit the State website beginning at 8:00am on Friday, January 22, 2021 to schedule your vaccination. https://www.vaccines.nh.gov
- If you are a New Hampshire resident, 65 years of age and younger with 2 or more high risk health conditions, (refer to list above) NOT an LRGH patient AND DO NOT HAVE a Primary Care Provider (PCP): Please contact 2-1-1
IT IS OUR GOAL THAT APPOINTMENTS WILL BEGIN STARTING JANUARY 27 AND WILL DEPEND ON THE AVAILABILITY OF THE VACCINE AS IT IS DISTRIBUTED BY THE STATE.
Additional Information:
- Depending on the distribution of vaccines from the State, it is our plan to have vaccines administered at Franklin Regional Hospital and Lakes Region General Hospital – on different days of the week.
- When you arrive at LRGHealthcare further directions will be provided concerning locations, time, COVID-19 protocols including masks, screening, parking and setting up second appointment for second dose.
- When you contact vaccines.nh.gov please be prepared to answer questions about allergies, medications. You will also be asked about health insurance – IT IS NOT REQUIRED INFORMATION, there is no charge for the vaccinations.
We know you have many questions and we will do our best to answer them as quickly as possible. New information about vaccine distribution is continuing to be released, and we appreciate your understanding and patience.
We will continue to update our website as we learn more.
If you have further questions about the State of New Hampshire plans please call the state hotline 2-1-1 at any time, or visit https://www.vaccines.nh.gov
RECOMMENDED RESOURCES ABOUT THE VACCINE:
COVID-19 Vaccine Information
We are encouraged with the news that COVID-19 vaccines have been approved for distribution across the country. LRGHealthcare is currently working on plans for the COVID-19 vaccination distribution to our staff and community. The State of NH is distributing this vaccine in a phased-in approach with the first group going to at-risk health corkers, residents of long-term care facilities and first responders.
We understand that you might have questions about the vaccine and we hope to be able to answer those questions as we continue the planning process. We are in the early stages of planning and will continue to update you as more information is available. Please check our website often as the latest information on the vaccine and distribution plans will be updated there.
Current Information
- The vaccine will require two doses, given 21 or 28 days apart depending on the vaccine. Both doses will be required for the vaccine to be effective.
- Supply of the vaccine is limited, however over the next couple of months we hope that most high-risk groups will have an opportunity to be vaccinated.
- More information on the vaccine and when you might be able to expect to get yours will be posted as we move forward.
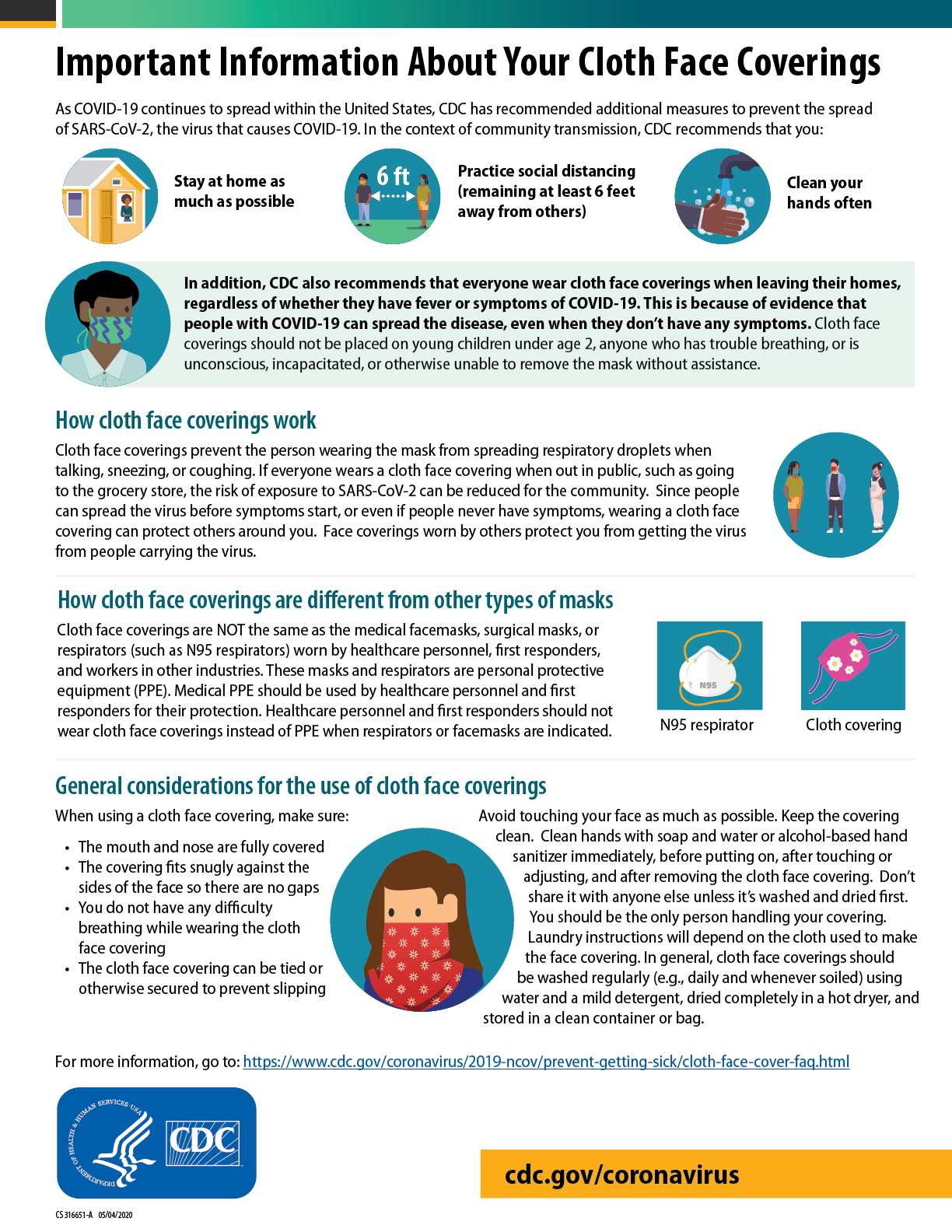
Help to limit the spread of COVID-19 by:
- Washing your hands often with soap and water for at least 20 seconds especially after you have been in a public place, or after blowing your nose, coughing, or sneezing.
- Practice social/physical distancing
- Cover your mouth and nose with a mask when around others
- Monitor your health daily
On Friday, Dec. 11, 2020, the FDA issued an Emergency Use Authorization (EUA) for the Pfizer COVID-19 vaccine. The EUA allows the use of the vaccine for individuals 16 years of age or older. Other manufacturer vaccines, such as Moderna, AstraZeneca, Janssen, and Novavax are in various stages of development, but only the Pfizer COVID-19 is currently available for use. Expected delivery dates, as well as numbers of doses to be delivered, are changing on a daily basis. We are committed to updating you about availability as information is confirmed.
Initial vaccine supply will be limited so not everyone will be able to be vaccinated right away. The COVID-19 vaccine will be given first to people at highest risk of infection including health care personnel and residents of long-term care facilities. Prioritization guidelines are in development for workers in essential and critical industries, people at high risk for severe COVID-19 illness due to underlying medical conditions, and people 65 years and older.
Herd immunity, or community immunity, occurs when a high percentage of the community is immune to a disease through vaccination and/or prior illness. Community immunity makes the spread of the virus from person to person unlikely. The CDC is still determining what percentage of the population in the US needs to be vaccinated to achieve community immunity.
COVID-19 mRNA vaccines (such as the Pfizer vaccine) are given in two doses, injected into the muscles of the upper arm, similar to a flu shot (intramuscularly).
The first shot starts building immunity, but it is not enough for protection. The second shot given a few weeks later is needed to get the most protection from the vaccine.
Pfizer’s vaccine is a 2-dose intramuscular injection separated by 21 days.
Moderna’s vaccine is a 2-dose intramuscular injection separated by 28 days. (The Moderna vaccine has not yet received Emergency Use Authorization by the FDA, but the FDA regulatory review process is underway.)
Yes. The COVID-19 vaccine products are not interchangeable; the second dose must be from the same manufacturer as your first dose.
When you receive your first dose, you will also receive a COVID-19 vaccination record card. Bring your COVID-19 vaccination record card when you return for your second dose to ensure you are getting the appropriate vaccination. You should be sure to return to the same location where you received your first dose.
The data from clinical trials indicate that the Pfizer and Moderna vaccines are safe. Both vaccines have undergone extensive clinical trials that tested for safety and efficacy before being submitted to the FDA for Emergency Use Authorization.
Common side effects include
- injection site pain, swelling, or redness
- tiredness
- feeling unwell
- headache
- muscle pain
- chills
- joint pain
- fever
- nausea
- swollen lymph nodes (lymphadenopathy)
Before being vaccinated, you will receive a COVID-19 Vaccine Emergency Use Authorization (EUA) Fact Sheet which will include important information about the vaccine. Be sure you read this Fact Sheet carefully.
If you experience a severe allergic reaction, call 9-1-1 or go to your nearest hospital.
If you believe you are having an adverse reaction, you should contact your health care provider and seek medical attention immediately. Adverse events following vaccination should be reported through the Vaccine Adverse Event Reporting System (VAERS) (1-800-822-7967 or through their website).
The CDC is implementing a new smartphone-based tool called v-safe to check-in with people about side effects after they receive a COVID-19 vaccine. When you receive your vaccine, you should also receive a v-safe information sheet telling you how to enroll in v-safe. If you enroll, you will receive regular text messages directing you to surveys where you can report any problems or adverse reactions you have after receiving a COVID-19 vaccine.
No, the vaccine does not contain any live virus.
Due to the current limited supply of vaccine, you will not be able to choose a specific vaccine manufacturer at this time.
The CDC states that it cannot comment on whether people who had COVID-19 should get a COVID-19 vaccine. There is not enough information currently available to say if, or for how long, after infection someone is protected from getting COVID-19 again.
The Emergency Use Authorization Fact Sheet for Pfizer COVID-19 vaccine states that if you are pregnant or breastfeeding, you should discuss your options with your health care provider. As pregnant women were not included in the Pfizer COVID-19 vaccine clinical trials, there is not enough data to know if the vaccine is safe for pregnant or lactating women.
We recommend that pregnant and lactating women contact their health care provider to discuss the current information available and each women’s individual circumstance before making a decision about receiving the vaccination.
If you have had a severe allergic reaction after a previous dose of this vaccine, or if you have had a severe allergic reaction to any ingredient in the vaccine, the Emergency Use Authorization Fact Sheet states that you should not get the Pfizer COVID-19 vaccine. We recommend that individuals with a history of anaphylaxis (severe, potentially life-threatening allergic reaction) consult their health care provider on making the decision as to whether or not to be vaccinated.
New Hampshire public health officials recommend administering the COVID-19 vaccine and flu vaccine on separate days. This limits any potential interaction between the two vaccines that may impact effectiveness. State-run vaccine clinics will not be offering the two vaccines on the same day.
Flu vaccination is encouraged for people who have not already received their annual flu vaccine. The flu vaccination is critical to reduce instances of flu in your community. Reducing flu cases also reduces the number of people seeking care for respiratory illness. This effort directly helps reduce the strain on the health care system during COVID-19 pandemic. Timing of flu vaccine and COVID-19 vaccine should be discussed with your primary care provider.
Yes. While experts learn more about the protection that COVID-19 vaccines provide under real-life conditions, it is important for everyone to continue covering your mouth and nose with a mask, washing hands often, and staying at least 6 feet away from others.
Together, COVID-19 vaccination and following the CDC’s recommendations for how to protect yourself and others will offer the best protection from getting and spreading COVID-19.
Based on manufacturer data, Pfizer’s vaccine was found to be 94.6% effective against COVID-19 beginning 7 days after the second dose.
Based on manufacturer data, Moderna’s vaccine was found to be 94.1% effective against COVID-19 after receiving two doses and 100% effective against severe COVID-19 disease.
No, not as a result of the vaccine alone. The vaccines won’t cause you to test positive on viral tests. If your body develops an immune response, which is the goal of vaccination, there is a possibility you may test positive on some antibody tests.
No. The antibody tests currently in use will generally only detect the type of antibody that is produced by a natural infection, not antibodies produced by a response to vaccination. Experts are currently looking at how COVID-19 vaccination may affect antibody testing results.
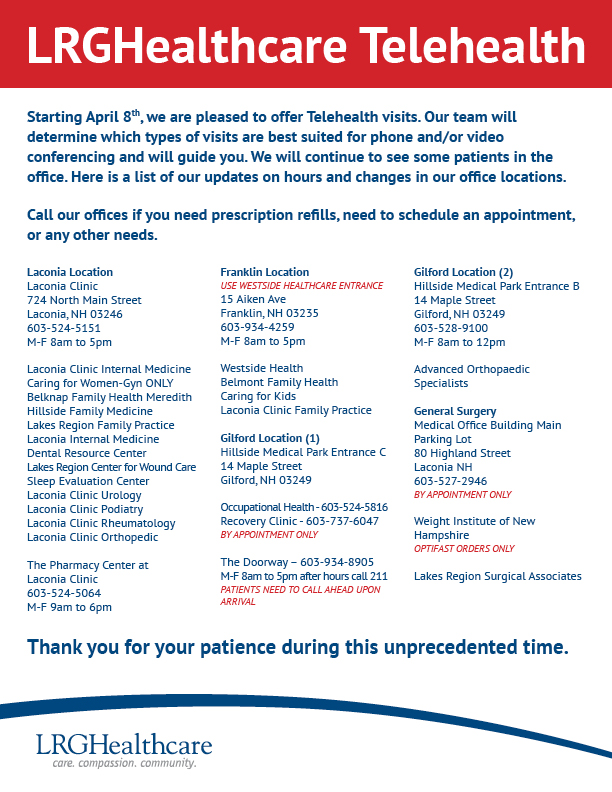
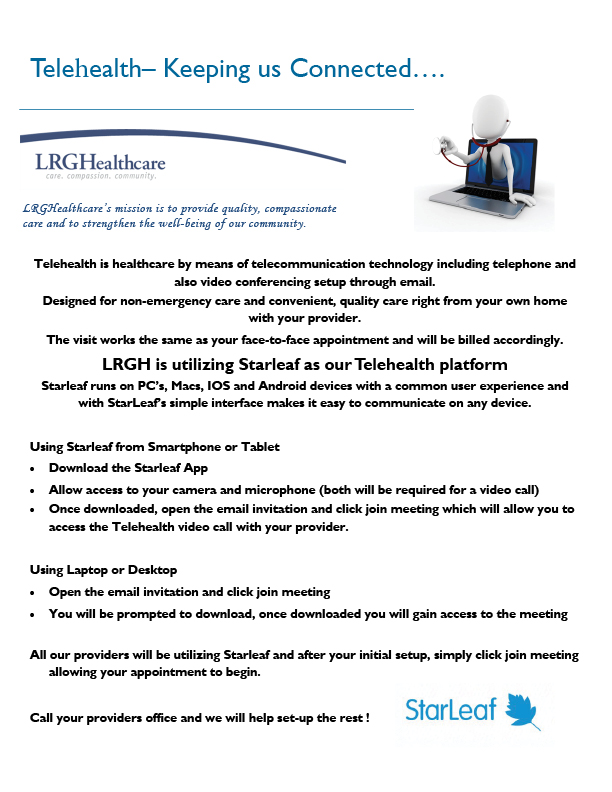
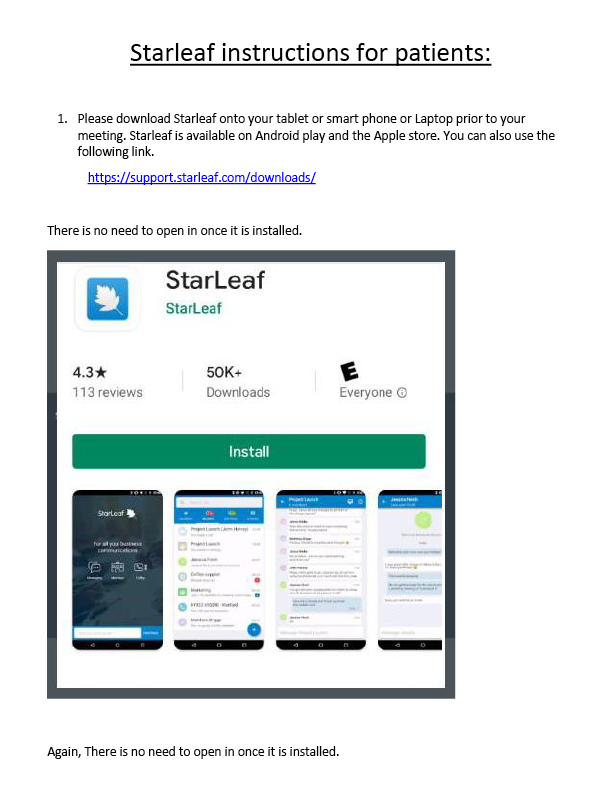
Lakes Region General Hospital and Franklin Regional Hospital, in our continued partnership with ClearChoiceMD, have created a strong network of healthcare services to our combined communities.
During our current COVID-19 pandemic our partnership and shared resources are even more important. Please know we are here for our communities.
As it relates to Community-based COVID-19 testing:
Depending on the individuals symptoms and if they have a Primary Care Provider (PCP) the following is a guide as to how our community members can expect to acquire a COVID-19 test.
- For asymptomatic individuals with PCPs, we direct patients to our partner, ClearChoiceMD, to receive testing at one of two locations in Belmont and Tilton. Quest testing is used in this scenario. Results are provided by ClearChoiceMD physicians to the patient.
- For symptomatic or asymptomatic individuals without PCPs, we direct patients to our partner, ClearChoiceMD, to receive testing at one of two locations in Belmont and Tilton. Quest testing is used in this scenario. Results are provided by ClearChoiceMD to the ordering physician.
- For symptomatic or asymptomatic individuals in either Lakes or Franklin hospital facilities (regardless of PCP status), we collect samples in the inpatient setting of Lakes. The State lab and Abbot rapid testing capabilities are used in this scenario. Results are provided by Lakes and the State to the ordering physician
Contact Information:
Lakes Region General Hospital
80 Highland St
Laconia, NH 03246
Main Number: 603-524-3211
Franklin Regional Hospital
25 Aiken Ave
Franklin, NH 03235
Main Number: 603-934-2060
COVID-19 Hotline: 603-527-7069
ClearChoiceMD
Belmont, NH
96 Daniel Webster Hwy
Belmont, NH 03220
Tilton, NH
75 Laconia Rd.
Tilton, NH 03276
Guidance on Universal Masking
Effective April 6, 2020, all visitors and staff entering any LRGHealthcare facility will be required to wear a cloth mask while in the facility. After screening of symptoms, a cloth mask will be handed out upon entry to the facility. Cloth masks will be collected from visitors and staff exiting the facility for washing and re-use.
Rationale for Masking Guidance:
- Act as a barrier to prevent touching of one’s face in the event one’s hands have become contaminated.
- Protect our patients and other staff members should the healthcare worker have early COVID-19 infection or develop symptoms at work.
- It’s important to note that universal masking is NOT designed to protect an individual from exposure to others who are sick; but instead is intended to protect others from possible exposure from the person wearing the mask. Universal masks contain the wearer’s respiratory droplets, helping to prevent them from landing on surfaces (such as computers or desks) or other people.
To be successful, this approach will require the following:
- Strict adherence to extended use/reuse of masks.
- Meticulous adherence to hand hygiene (including before and after removing masks).
- Proper mask use and hygiene including wearing the mask as directed to cover the mouth and nose.
- Strict avoidance of manipulation/touching the mask to reduce the risk of contamination and self-inoculation.
- Adherence to the principle of social distancing as much as possible (i.e. allow 6 feet distance from others).
Infection Prevention Guidance on Procedure/Surgical and Cloth Mask Use and Re-Use
To remove facemask with intent to reuse:
- Perform hand hygiene before removing facemask.
- Remove mask
- Ear-Loop Mask Style: Remove mask by holding the ear loops. Remove slowly and carefully. Avoid touching either side of the mask.
- Tie Back: Remove mask by untying lower ties FIRST. Untie upper ties last. Remove slowly and carefully. Ensure ties do not fall into either side of mask. Avoid touching either side of the mask.
- After removing mask, visually inspect for contamination, distortion in shape/form. If soiled, torn, or saturated the mask should be discarded.
- If the mask is NOT visibly soiled, torn, or saturated, carefully store in a paper bag (label with your name, and “front” and “back” on the two sides). Insert mask so that the front of the mask faces the side of the bag labeled “front.”
- Perform hand hygiene after removing facemask.
To re-apply used mask:
- Perform hand hygiene before re-applying mask.
- Grasp mask
-
- Pinch mask at the ear loops or grasp upper ties.
- Place over face
- For ear-loop style mask: Secure ear loops behind the ears. Secure mask.
- For tie back style mask: Secure upper ties first, behind head. End by securing lower ties behind head.
- Perform hand hygiene after re-applying mask.
- This guidance is NOT applicable to any healthcare personnel involved in the care of patients on Droplet or COVID-19 Precautions. For those cases, if you are wearing your own supply of surgical mask or a cloth mask, it should be doffed and stored in a brown paper bag and a surgical mask obtained as part of the expected PPE for the patient visit. Use N-95 respirators for patients on Airborne Precautions.
Frequently Asked Questions
Will LRGHealthcare provide the surgical/procedure masks for Universal Masking? NO. Due to limited supply of surgical/procedure mask, this is only provided for healthcare personnel involved in the care of patients on Droplet or COVID-19 Precautions or involved in procedures requiring surgical/procedure mask. LRGHealthcare will be able to provide homemade cloth masks that are generously donated by the community.
Can I use my own mask or respirator? YES, as long as Infection Control Guidance on Procedure/Surgical and Cloth Mask Use and Re-use is strictly followed. It is important to understand that a cloth mask is NOT considered PPE and masks/respirators brought from home may not be FDA approved for PPE use. When caring for a patient on droplet or COVID-19 precautions, we recommend the use of hospital supplied surgical/procedure mask.
Can a single procedural mask be worn continuously, including across different cases? Yes, a single mask can be worn between different patients with the exception of care of patient on Droplet or COVID-19 Precautions. For those cases, if you are wearing your own supply of surgical mask or a cloth mask, it should be doffed and stored in a brown paper bag and a surgical mask obtained as part of the expected PPE for the patient visit. Use N-95 respirators for patients on Airborne Precautions.
I work in a clinical setting. How can I eat/drink when I am supposed to wear a mask? Perform hand hygiene, remove the mask, eat or drink in an approved location, and then replace your procedure/surgical mask or cloth mask. Please follow the guidelines on appropriate doffing.
Sewing Masks for Donations
One way to supplement our ever-changing inventory of Personal Protective Equipment (PPE) is to join the national movement of volunteers who have started to sew masks. This generous outpouring is in response to the Center for Disease Control’s guidance that fabric masks are a crisis response option when other supplies have been exhausted.
Below is our general guidance for those who wish to participate and help by sewing masks for donation.
Thank you for donating your time and talent to help LRGHealthcare. We appreciate your generosity.
Important infection prevention
Before starting this project, please ask yourself the following questions:
- Have you been in contact with anyone suspected or confirmed to have COVID-19 in the past 14 days?
- Do you have fever, cough or shortness of breath?
If you are able to answer “NO” to both questions, then proceed with making masks.
If you answer “YES” to either or both questions, please do not make masks. If you are experiencing cough, fever, or shortness of breath and have a concern that you may have COVID-19 please call your primary care provider for a risk assessment.
Instructions for making masks
Materials
- 100% unused cotton fabric (front) – no metallic fabrics
- 100% cotton or cotton flannel (back)
- 1/4″ or 3/8” flat elastic
An instruction video is available from Deaconess Health System.
Written instructions are also available.
Dropping off masks
Masks can be dropped off in a re-sealable plastic bag at a bin located at the entrance of LRGHealthcare, 80 Highland Street, Laconia, NH. Please include your name, email address or phone number so we can kindly acknowledge your assistance.
LRGHealthcare Press Release
FOR IMMEDIATE RELEASE
April 3, 2020
Laconia, NH – LRGHealthcare Response to COVID-19 Crisis from Kevin W. Donovan, President and CEO
LRGHealthcare is closely monitoring the coronavirus disease (COVID-19) outbreak and preparing for any possible disruptions, as well as supporting public health agencies to help the community prepare. A major first preparation step for the organization was cancellation of all elective and non-urgent surgeries, procedures and outpatient visits a few weeks ago.
In further preparation and due to the economic impact of the COVID-19 crisis, effective on or about April 7th, LRGHealthcare will take the following short-term steps to ensure we can effectively respond to the expected surge in COVID-19 cases in our community.
- Temporarily close most outpatient services including Doctor’s offices
- Downsize non-clinical areas
- Maintain minimal Medical Staff to support essential COVID-19 activities
- Furlough approximately 500 full-time equivalent employees
These temporary changes will allow us to focus our efforts on the COVID-19 response and maintain Lakes Region General Hospital and Franklin Regional Hospital’s core hospital services.
Today, Governor Sununu announced that the state has approved a $5.25 million interest free loan that will greatly support the organization in the coming days and weeks as this situation evolves. We are grateful for the support Governor Sununu has extended to LRGHealthcare. We expect, with this support and with the temporary changes we’ve announced, we will meet the needs of our community during this pandemic.
We also want to reassure our community that LRGHealthcare has continued, despite the current crisis to be on a strong footing to finalize plans with a partner in the future.
LRGHealthcare is setting up a fund for our furloughed employees to lessen the impact of being displaced during these trying times. We will keep their healthcare benefits in place, but they would benefit from other financial support at this time.
The LRGHealthcare COVID-19 Hotline (603-527-7069) is available DAILY from 7am-7pm, to answer your questions. You can also visit our website at LRGH.org for up-to-date information.
LRGH COVID-19 RESPONSE FUND
We know these are difficult, and even scary times for you. The world is facing an unprecedented challenge with communities and economies everywhere affected by the growing COVID-19 pandemic. Our community is coming together to help us combat the COVID-19 pandemic bringing much needed supplies to help us respond to this outbreak. The outpouring of support has been amazing.
As you are aware, we have undertaken steps to put us in a position to fight this pandemic, including suspending non-emergent surgeries and services in order to open up hospital beds in anticipation of a surge of critically ill patients. All these steps have led to a 54% decrease in our revenue stream. Your help is important as we move forward, caring for our community’s traumatic and emergent illnesses in addition to COVID-19.
Donations received can go towards funding:
- COVID-19 Operations which include buying essential supplies such as masks, gloves and protective wear for frontline workers
- COVID-19 Employee Assistance Fund which will help ensure employees get the assistance they need until they are back at work
Your donation is greatly appreciated in our effort to respond to COVID-19, especially when the needs are greatest and resources are lowest. Thank you.
Click here to donate: https://concordhospital-laconia.org/giving/
Sewing Surgical/Scrub Caps for Donations
Supplies needed:
– 1/3 yd of Main Fabric of your choosing. (If 44 inches wide, should be enough for both pieces)
– Accent Fabric (or scrap fabric) that is at least 8 1/2 by 11 inches
– 1/2 inch wide Elastic Band
– Ruler and/or Measuring Tape
– Pins
– Scissors
– Sewing Machine and Thread
– Iron/Ironing Board
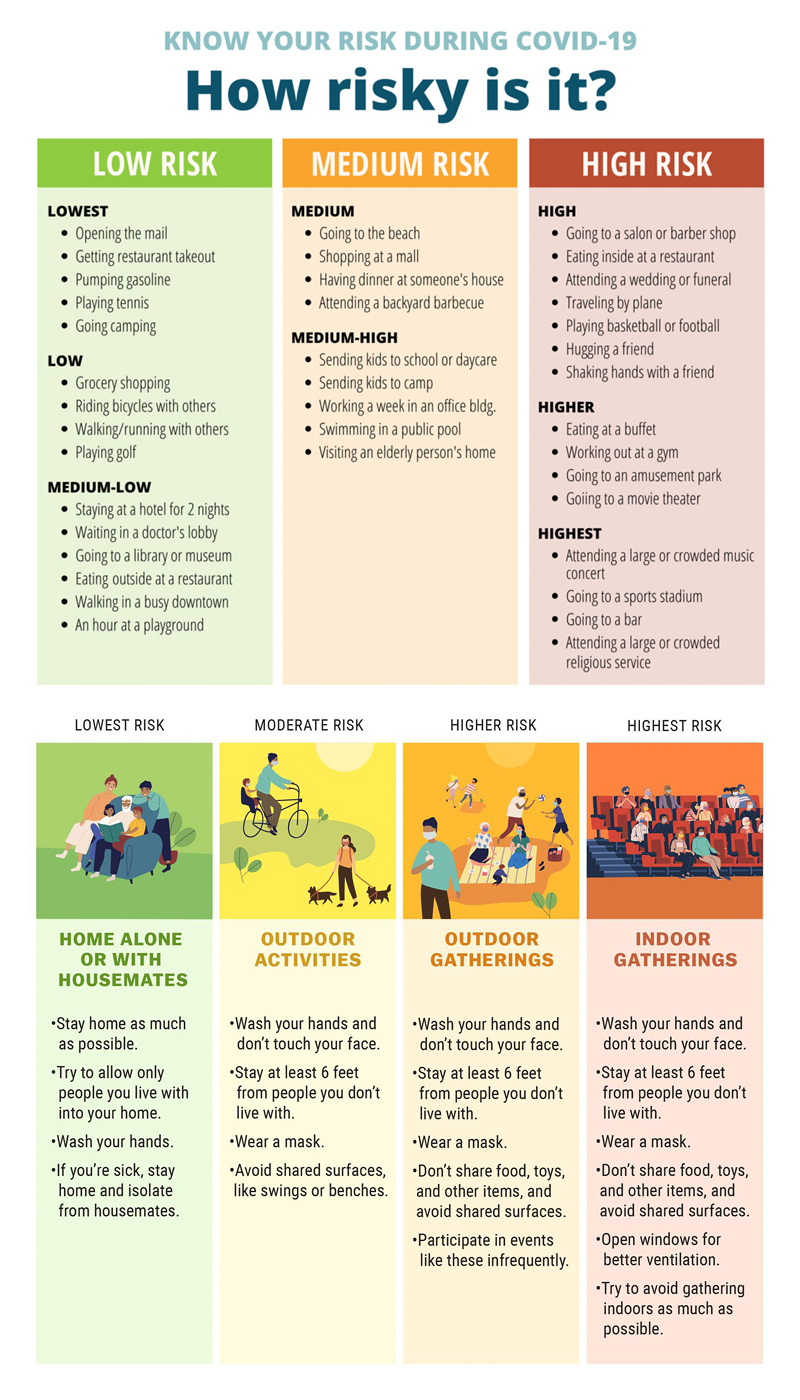
Step 1: Cutting the Fabric
You will need to cut out two pieces of fabric. One of for the main body of the hat and one for the top. (Use the iron to help flatten out the kinks and folds in the fabric before cutting.)
For the main body of the hat, cut a rectangular piece of fabric with the dimensions 12 x 30 inches.
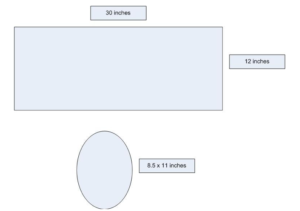
For the top of the hat, I created a pattern using one 8 1/2 x 11 sheet of paper. Make sure that one end of the fabric is flat.
Step 2: Sewing
Main body fabric = MainF
Top fabric = TopF
**Sew all edges with 1/4 inch seam**
A. Take MainF and fold it hot dog style with the wrong sides touching. Using the iron, flatten the fold along the bottom. Flipping the fabric inside out, sew along the two ends of the fabric, leaving the top open. After sewing the ends closed, flip the fabric right side out again. Iron the ends flat.
B. Take the closed end of MainF and create a 1 1/2 inch flap. Iron the fold.
C. Create an overlap with the two ends of about 2 1/2 inches. Sew both ends down.
D. With the fold facing the outside, fold MainF in half with the thick end on the left. Fold TopF in half with the flat portion facing towards you. Line up the two fabrics right sides together. Pin together along the edge of the entire hat, leaving the flat portion of TopF unpinned.
E. This is the trickiest part. When you get to the flat portion of the fabric, pin the middle of TopF to the middle of thick portion of MainF. Flag the extra fabric and sew this extra portion down. If confused, please refer to the pictures.
F. Sew MainF and TopF together leaving a 1/4 seam along the edge.
Step 3: Adding the Elastic Band
After sewing the two portions together, flip the hat. The folded flap should be on the outside now.
Cut about a 6 inch long piece of elastic band. Start with either the left or right side of the thick portion of the hat. About 4 inches from the edge, sew the elastic down on the inside of the flap. Sew down the flap to the fold and along the edge to the other side. Close up the gap by sewing down the other end of elastic 4 inches from the other side. After releasing the hat, it should scrunch together.
Note: If you feel the hat is still too loose, you can either shorten the length of the elastic or sew further out from the middle of the hat.
Step 4: Reaping the Compliments
Final outcome: One Awesome looking surgical/scrub cap.
Check out this video for more help – https://www.instructables.com/id/DIY-SurgicalScrub-Hat/
At AHA Press Briefing, Hospitals Describe Dire Need for More Federal Funding to Fight Pandemic and Care for Patients and Communities
At an AHA press briefing today, hospital and health system leaders from across the country described the urgent need for federal aid to ensure that frontline medical personnel have the tools and resources they need to effectively respond to the COVID-19 crisis.
“We’ve already seen facilities facing shortages of needed equipment and high expenses in providing critical care and this hurts our country’s ability to respond,” said AHA President and CEO Rick Pollack. “…The reality is that we are in a war in which hospitals and health systems are on the frontlines and our health care workers are putting their lives on the line to fight this battle … No one ever sends their troops into battle without the right protection and ammunition and tools.”
The AHA, American Medical Association and American Nurses Association Thursday urged congressional leaders to provide $100 billion to front line health care personnel and providers and direct federal agencies to infuse funds immediately so they can take the necessary steps to fight the pandemic.
Pollack also emphasized the need for having enough tests and getting the test results as quickly as possible in order to have a more accurate picture of the infection rate.
“Ensuring the safety of the patients, protecting health care workers and supporting the health and safety of our community is what we’re all about, and it requires every part of the health care sector to work together, from those on the front lines to the federal, state and local government,” Pollack said. “Equipped with the right tools, guidance and resources we will do our very best to protect lives and keep people healthy.”
Scott Graham, CEO of Three Rivers and North Valley Hospitals in rural Washington state said, “We’re trying to figure out how to stay in business.” Because of the mandates for social distancing and state’s cancellation of elective surgeries, he said “the revenue that typically comes in that we need to cover the cost of operating has dried up. …we are now in a negative cash position and are using credit. We will exhaust all avenues to make payroll in the next three or four weeks.”
Even before the COVID-19 crisis, One Brooklyn Health System in New York was relying on more than $20 million a month in support from New York State to keep its safety net hospitals open, said LaRay Brown, its president and CEO. “We had less than two weeks cash on hand before COVID-19,” she said. “We are now looking at an additional cost of $30-$34 million a month from projected staff increases to cover surge capacity” and replace staff who are on furlough, self-isolating or must care for their children while city schools are closed.
Kevin Donovan, president and CEO of LRGHealthcare in central New Hampshire, projects his health system’s freeze on elective services during the public health crisis will cost at least $50 million. “Prior to this crisis, much like my colleagues, we were in extremely poor financial condition,” he said, with “only a handful of cash on hand” and no debt capacity to borrow money.
“I think these stories are reflective of the experiences of thousands of hospitals across the country,” Pollack said. “That’s why the legislation being considered on the Hill right now is so important in terms of providing needed support.”
LRGH COVID-19 Hotline
During normal business hours we encourage you to contact your Primary Care Provider (PCP) or the Hotline.
The LRGH Covid-19 hotline (603-527-7069) is available for patients to call DAILY 7am-5pm to answer your questions. It is staffed with a nurse who can help triage symptoms you may be experiencing and provide you guidance for further follow up. You can also visit our website at www.concordhospital-laconia.org for up to date information.
After normal business hours If you are concerned that you may have Covid-19 symptoms, please call the State Public Health Department at 603-271-4496. If you are experiencing a medical emergency, please call 911 or go to your nearest emergency department.
We Can All Do Something to Help
The COVID-19 pandemic is scary, and it’s natural to feel overwhelmed by what is going on. Unfortunately, the reality is that things will get a lot worse in the coming weeks and months, and many people in our communities are going to need help. The good news is that there are things you can do today to change the course of the pandemic and help our community get through it.
1. Social Distancing: This is by far the most important thing you can do to help our community, not to mention to protect yourself and your family. Please share these resources with anyone you know who is skeptical about having to stay home.
Why outbreaks of coronavirus spread exponentially, and how to “flatten the curve” –Washington Post
Social Distancing: This is not a snow day – Medium.com
COVID-19 is different from flu, and we must respond differently – CNN
2. Food Supports: Donate to a Got Lunch organization in your town and to your local food pantry.
Yesterday, the Governor announced that schools are closed, but that they will distribute food to families whose children participate in their school’s food programs. We know that local Got Lunch! organizations have been mobilizing to distribute groceries to families during this crisis. Both will be a big help to families who are losing income due to the pandemic.
Food pantries will help elderly or disabled residents of low-income and families who don’t have a Got Lunch program in their town.
You can also offer to go get groceries for your relatives and neighbors who are over the age of 60 or have underlying health problems. These people should be self-isolating at home – it is dangerous for them to go anywhere.
3. Support Local Businesses: You can stay home while still spending money at your favorite local businesses by buying gift certificates to use later. The vast majority of businesses in our region and state are small and locally owned and they will be hit hard by this crisis. The more we support them, the more they can support their employees during this difficult time.
The days ahead will be challenging. But we are not helpless in the face of this pandemic. Each of us has the power change the course of history with our choices over the coming weeks and months. There is a strong spirit of generosity and community here in the Lakes Region – we have a lot of practice giving back and helping out! So I know that, while we may all experience sadness in the days to come, we will also feel moments of great hope as we work together to overcome this unprecedented challenge.
Yours in hope and community,
Carmen R. Lorentz
Visitation Policy/Message COVID 19
Message to our community
Out of an abundance of caution, LRGHealthcare will restrict all visitors to Franklin Regional Hospital, Lakes Region General Hospital, and all affiliates of LRGHealthcare, effective Noon, Sunday, March 15, 2020.
We are taking this measure to protect our patients and employees from potential exposure to Coronavirus (COVID-19).
In addition to this temporary visitation policy, we are suspending all community meetings held on premises, community education classes and community access to our cafeterias.
If you have a loved one who is critically ill and it is imperative that you see them, please call 603-524-3211 to contact a hospital leadership representative on call. Requests will be reviewed on a case by case basis.
PLEASE NOTE: During this restricted visitation time, if you want to have patients receive a delivery of flowers, our staff will ensure that they receive them.
Thank you for your continued commitment to keep our community healthy.
The New Hampshire Department of Health and Human Services has developed a website just for COVID-19 information.
State Launches 2-1-1 COVID-19 Hotline
CONCORD, NH – Today, Governor Chris Sununu, the New Hampshire Department of Health and Human Services, and NH Homeland Security and Emergency Management, announced that 211NH has been mobilized to handle all COVID-19 related calls from New Hampshire residents. All residents with questions or concerns surrounding the COVID-19 outbreak can call 2-1-1.
“211NH will serve as a coordinated and streamlined process for any Granite Stater concerned about the coronavirus,” said Governor Chris Sununu. “Now that it is up and running, any New Hampshire residents can call with questions or concerns. I would like to thank the folks at Granite United Way and Public Health for working around the clock to stay on top of this evolving public health situation by making this critical resource available 24/7.”
“It is important during an outbreak that residents get the information they need to protect their health and the health of their community,” said HHS Commissioner Lori Shibinette. “2-1-1 provides that resource for our residents to get the most up to date and accurate information about the presence of coronavirus in New Hampshire.”
211NH is New Hampshire’s statewide, comprehensive, information and referral service operated by Granite United Way and will replace the current Department of Public Health Hotline (603-271-4496) for COVID-19 related questions.
Members of the media and local city and town officials, as well as emergency management officials should still call the state’s Joint Information Center.
LRGH COVID-19 Hotline
During normal business hours we encourage you to contact your Primary Care Provider (PCP) or the Hotline.
The Covid-19 hotline (603-527-7069) is available for patients to call Monday-Friday 8am-4pm to answer your questions. It is staffed with a nurse who can help triage symptoms you may be experiencing and provide you guidance for further follow up. You can also visit our website at www.concordhospital-laconia.org for up to date information.
After normal business hours If you are concerned that you may have Covid-19 symptoms, please call the State Public Health Department at 603-271-4496. If you are experiencing a medical emergency, please call 911 or go to your nearest emergency department.
Thank you!
Fact sheet:
Coronavirus disease 2019 (COVID-19)
What it is
Coronavirus disease 2019 (COVID-19) is a respiratory illness which was first identified in Wuhan, Hubei Province, China.
How it spreads
The CoVID-19 virus is spread from person-to-person, although the CDC does not yet know how easily it is spread between people.
The scope of the problem
- COVID-19 has spread to other countries, with significant outbreaks in South Korea and sustained cases of community transmission in Iran, Italy and Japan, according to the CDC.
- There are more than 81,000 confirmed cases worldwide and more than 3200 deaths.
- There have been 60 confirmed cases in the United States (see https://www.cdc.gov/coronavirus/2019-ncov/cases-in-us.html for the most updated case count).
- As of March 4th, two patients in NH have tested (presumptive) positive for COVID-19 and others are undergoing testing.
How LRGHealthcare is Prepared
- With guidance from the NH DHHS, we have plans in place to manage patients with COVID-19 while safeguarding patients, hospital visitors, health care workers and the community at large.
- Travel screenings are in place for all intake staff to identify higher risk patients.
- If a patient tests positive for the illness, the appropriate protocol is already in place, including isolation of the patient in an Airborne Isolation room.
What the Public Should Do
- Because it is currently the cold and flu season, the CDC recommends getting the flu vaccine if you have not already. Influenza symptoms can mimic COVID-19 symptoms.
- Individuals should continue to exercise standard safety measures, including not touching your eyes, nose and mouth with unwashed hands.
- Wash your hands often with soap and water for at least 20 seconds, especially after using the bathroom; use an alcohol-based hand sanitizer if soap and water are not available. (In most circumstances, alcohol-based hand sanitizers are highly effective alternatives to soap and water for health care providers in the workplace.)
- Do not go to work if you are sick and do not send your children to school if they are sick.
- If you are sick and have traveled to a region where COVID-19 is spreading, or have been in contact with someone suspected of having COVID-19, call your health care provider immediately for recommendations on how best to be evaluated; do not go to a hospital, urgent care site, or outpatient clinic without calling ahead to report your travel history.
The Symptoms
The main symptoms of the illness include fever, dry cough, shortness of breath and myalgia. The symptoms may appear in as few as two days or as many as two weeks after exposure.
Severity of the illness
COVID-19 can cause severe illness in some people, including death, although, based on preliminary information, the World Health Organization has stated that a large majority (82%) of COVID-19 cases have been mild; approximately 3% have been critical.
Treatment and Prevention
- There is currently no vaccine available for COVID-19. Vaccine development is in progress.
- There is currently no specific antiviral treatment recommended for COVID-19. Research studies assessing potential treatments are in progress.
Current CDC Travel Warnings
- The CDC has issued travel warnings to U.S. residents, recommending that all travelers avoid all nonessential travel to China, Iran, Italy and South Korea.
- Additionally, the CDC is advising that older adults and those with chronic medical conditions consider postponing nonessential travel to Japan, as that country is experiencing sustained community spread of COVID-19.
- Before traveling to any country, the CDC advises that you visit cdc.gov/coronavirus/2019-ncov/travelers/index.html to see the current risks and advisories.
Current LRGHealthcare Travel Advisory
- LRGHealthcare strongly discourages employees from traveling to any CDC Warning level 3 and Alert level 2 country. This is a rapidly evolving situation; additional countries may be added to the CDC travel advisory list as circumstances change.
For Additional Information
- LRGHealthcare actively monitoring COVID-19 and has a helpful website for faculty and students.
- Visit the CDC website for updates on COVID-19 including current travel warnings and alerts.
The New Hampshire Department of Health and Human Services (DHHS) and the Division of Public Health Services (DPHS) announced the first presumptive positive test result in New Hampshire for COVID-19, the disease caused by the new coronavirus today.
State Epidemiologist Dr. Benjamin Chan said, “This positive test is in an individual who traveled to Italy and developed symptoms consistent with COVID-19 within several days of travel. At this time, there is no evidence of more widespread community transmission in New Hampshire.”
The NH Public Health Laboratories (PHL) conducted the test and identified the presumptive positive result. The patient’s specimen is being sent to the Center for Disease Control (CDC) for confirmatory testing. The CDC is conducting confirmatory tests on all state laboratory tests that are found to be presumptively positive for COVID-19.
Because COVID-19, and all respiratory illnesses, are most commonly spread through respiratory droplets, residents should take the same precautions as those recommended to prevent the spread of influenza:
- Stay home and avoid public places when sick (i.e., social distancing)
- Cover mouth and nose when coughing and sneezing
- Wash hands frequently
- Avoid being within 6 feet (close contact) of a person who is sick
- Avoid sharing drinks, smoking/vaping devices, or other utensils or objects that may transmit saliva
- Disinfect frequently touched surfaces
We have convened a multi-disciplinary, Executive Steering Committee to assess the COVID-19 (Coronavirus) situation and determine our course of action moving forward.
LRGHealthcare is committed to keeping our community safe and apprised of the COVID-19 (Coronavirus) situation.
Guidance on Universal Masking
Effective April 6, 2020, all visitors and staff entering any LRGHealthcare facility will be required to wear a cloth mask while in the facility. After screening of symptoms, a cloth mask will be handed out upon entry to the facility. Cloth masks will be collected from visitors and staff exiting the facility for washing and re-use.
Rationale for Masking Guidance:
- Act as a barrier to prevent touching of one’s face in the event one’s hands have become contaminated.
- Protect our patients and other staff members should the healthcare worker have early COVID-19 infection or develop symptoms at work.
- It’s important to note that universal masking is NOT designed to protect an individual from exposure to others who are sick; but instead is intended to protect others from possible exposure from the person wearing the mask. Universal masks contain the wearer’s respiratory droplets, helping to prevent them from landing on surfaces (such as computers or desks) or other people.
To be successful, this approach will require the following:
- Strict adherence to extended use/reuse of masks.
- Meticulous adherence to hand hygiene (including before and after removing masks).
- Proper mask use and hygiene including wearing the mask as directed to cover the mouth and nose.
- Strict avoidance of manipulation/touching the mask to reduce the risk of contamination and self-inoculation.
- Adherence to the principle of social distancing as much as possible (i.e. allow 6 feet distance from others).
Infection Prevention Guidance on Procedure/Surgical and Cloth Mask Use and Re-Use
To remove facemask with intent to reuse:
- Perform hand hygiene before removing facemask.
- Remove mask
- Ear-Loop Mask Style: Remove mask by holding the ear loops. Remove slowly and carefully. Avoid touching either side of the mask.
- Tie Back: Remove mask by untying lower ties FIRST. Untie upper ties last. Remove slowly and carefully. Ensure ties do not fall into either side of mask. Avoid touching either side of the mask.
- After removing mask, visually inspect for contamination, distortion in shape/form. If soiled, torn, or saturated the mask should be discarded.
- If the mask is NOT visibly soiled, torn, or saturated, carefully store in a paper bag (label with your name, and “front” and “back” on the two sides). Insert mask so that the front of the mask faces the side of the bag labeled “front.”
- Perform hand hygiene after removing facemask.
To re-apply used mask:
- Perform hand hygiene before re-applying mask.
- Grasp mask
-
- Pinch mask at the ear loops or grasp upper ties.
- Place over face
- For ear-loop style mask: Secure ear loops behind the ears. Secure mask.
- For tie back style mask: Secure upper ties first, behind head. End by securing lower ties behind head.
- Perform hand hygiene after re-applying mask.
- This guidance is NOT applicable to any healthcare personnel involved in the care of patients on Droplet or COVID-19 Precautions. For those cases, if you are wearing your own supply of surgical mask or a cloth mask, it should be doffed and stored in a brown paper bag and a surgical mask obtained as part of the expected PPE for the patient visit. Use N-95 respirators for patients on Airborne Precautions.
Frequently Asked Questions
Will LRGHealthcare provide the surgical/procedure masks for Universal Masking? NO. Due to limited supply of surgical/procedure mask, this is only provided for healthcare personnel involved in the care of patients on Droplet or COVID-19 Precautions or involved in procedures requiring surgical/procedure mask. LRGHealthcare will be able to provide homemade cloth masks that are generously donated by the community.
Can I use my own mask or respirator? YES, as long as Infection Control Guidance on Procedure/Surgical and Cloth Mask Use and Re-use is strictly followed. It is important to understand that a cloth mask is NOT considered PPE and masks/respirators brought from home may not be FDA approved for PPE use. When caring for a patient on droplet or COVID-19 precautions, we recommend the use of hospital supplied surgical/procedure mask.
Can a single procedural mask be worn continuously, including across different cases? Yes, a single mask can be worn between different patients with the exception of care of patient on Droplet or COVID-19 Precautions. For those cases, if you are wearing your own supply of surgical mask or a cloth mask, it should be doffed and stored in a brown paper bag and a surgical mask obtained as part of the expected PPE for the patient visit. Use N-95 respirators for patients on Airborne Precautions.
I work in a clinical setting. How can I eat/drink when I am supposed to wear a mask? Perform hand hygiene, remove the mask, eat or drink in an approved location, and then replace your procedure/surgical mask or cloth mask. Please follow the guidelines on appropriate doffing.
Sewing Masks for Donations
One way to supplement our ever-changing inventory of Personal Protective Equipment (PPE) is to join the national movement of volunteers who have started to sew masks. This generous outpouring is in response to the Center for Disease Control’s guidance that fabric masks are a crisis response option when other supplies have been exhausted.
Below is our general guidance for those who wish to participate and help by sewing masks for donation.
Thank you for donating your time and talent to help LRGHealthcare. We appreciate your generosity.
Important infection prevention
Before starting this project, please ask yourself the following questions:
- Have you been in contact with anyone suspected or confirmed to have COVID-19 in the past 14 days?
- Do you have fever, cough or shortness of breath?
If you are able to answer “NO” to both questions, then proceed with making masks.
If you answer “YES” to either or both questions, please do not make masks. If you are experiencing cough, fever, or shortness of breath and have a concern that you may have COVID-19 please call your primary care provider for a risk assessment.
Instructions for making masks
Materials
- 100% unused cotton fabric (front) – no metallic fabrics
- 100% cotton or cotton flannel (back)
- 1/4″ or 3/8” flat elastic
An instruction video is available from Deaconess Health System.
Written instructions are also available.
Dropping off masks
Masks can be dropped off in a re-sealable plastic bag at a bin located at the entrance of LRGHealthcare, 80 Highland Street, Laconia, NH. Please include your name, email address or phone number so we can kindly acknowledge your assistance.
LRGHealthcare Press Release
FOR IMMEDIATE RELEASE
April 3, 2020
Laconia, NH – LRGHealthcare Response to COVID-19 Crisis from Kevin W. Donovan, President and CEO
LRGHealthcare is closely monitoring the coronavirus disease (COVID-19) outbreak and preparing for any possible disruptions, as well as supporting public health agencies to help the community prepare. A major first preparation step for the organization was cancellation of all elective and non-urgent surgeries, procedures and outpatient visits a few weeks ago.
In further preparation and due to the economic impact of the COVID-19 crisis, effective on or about April 7th, LRGHealthcare will take the following short-term steps to ensure we can effectively respond to the expected surge in COVID-19 cases in our community.
- Temporarily close most outpatient services including Doctor’s offices
- Downsize non-clinical areas
- Maintain minimal Medical Staff to support essential COVID-19 activities
- Furlough approximately 500 full-time equivalent employees
These temporary changes will allow us to focus our efforts on the COVID-19 response and maintain Lakes Region General Hospital and Franklin Regional Hospital’s core hospital services.
Today, Governor Sununu announced that the state has approved a $5.25 million interest free loan that will greatly support the organization in the coming days and weeks as this situation evolves. We are grateful for the support Governor Sununu has extended to LRGHealthcare. We expect, with this support and with the temporary changes we’ve announced, we will meet the needs of our community during this pandemic.
We also want to reassure our community that LRGHealthcare has continued, despite the current crisis to be on a strong footing to finalize plans with a partner in the future.
LRGHealthcare is setting up a fund for our furloughed employees to lessen the impact of being displaced during these trying times. We will keep their healthcare benefits in place, but they would benefit from other financial support at this time.
The LRGHealthcare COVID-19 Hotline (603-527-7069) is available DAILY from 7am-7pm, to answer your questions. You can also visit our website at LRGH.org for up-to-date information.
LRGH COVID-19 RESPONSE FUND
We know these are difficult, and even scary times for you. The world is facing an unprecedented challenge with communities and economies everywhere affected by the growing COVID-19 pandemic. Our community is coming together to help us combat the COVID-19 pandemic bringing much needed supplies to help us respond to this outbreak. The outpouring of support has been amazing.
As you are aware, we have undertaken steps to put us in a position to fight this pandemic, including suspending non-emergent surgeries and services in order to open up hospital beds in anticipation of a surge of critically ill patients. All these steps have led to a 54% decrease in our revenue stream. Your help is important as we move forward, caring for our community’s traumatic and emergent illnesses in addition to COVID-19.
Donations received can go towards funding:
- COVID-19 Operations which include buying essential supplies such as masks, gloves and protective wear for frontline workers
- COVID-19 Employee Assistance Fund which will help ensure employees get the assistance they need until they are back at work
Your donation is greatly appreciated in our effort to respond to COVID-19, especially when the needs are greatest and resources are lowest. Thank you.
Click here to donate: https://concordhospital-laconia.org/giving/
Sewing Surgical/Scrub Caps for Donations
Supplies needed:
– 1/3 yd of Main Fabric of your choosing. (If 44 inches wide, should be enough for both pieces)
– Accent Fabric (or scrap fabric) that is at least 8 1/2 by 11 inches
– 1/2 inch wide Elastic Band
– Ruler and/or Measuring Tape
– Pins
– Scissors
– Sewing Machine and Thread
– Iron/Ironing Board
Step 1: Cutting the Fabric
You will need to cut out two pieces of fabric. One of for the main body of the hat and one for the top. (Use the iron to help flatten out the kinks and folds in the fabric before cutting.)
For the main body of the hat, cut a rectangular piece of fabric with the dimensions 12 x 30 inches.
For the top of the hat, I created a pattern using one 8 1/2 x 11 sheet of paper. Make sure that one end of the fabric is flat.
Step 2: Sewing
Main body fabric = MainF
Top fabric = TopF
**Sew all edges with 1/4 inch seam**
A. Take MainF and fold it hot dog style with the wrong sides touching. Using the iron, flatten the fold along the bottom. Flipping the fabric inside out, sew along the two ends of the fabric, leaving the top open. After sewing the ends closed, flip the fabric right side out again. Iron the ends flat.
B. Take the closed end of MainF and create a 1 1/2 inch flap. Iron the fold.
C. Create an overlap with the two ends of about 2 1/2 inches. Sew both ends down.
D. With the fold facing the outside, fold MainF in half with the thick end on the left. Fold TopF in half with the flat portion facing towards you. Line up the two fabrics right sides together. Pin together along the edge of the entire hat, leaving the flat portion of TopF unpinned.
E. This is the trickiest part. When you get to the flat portion of the fabric, pin the middle of TopF to the middle of thick portion of MainF. Flag the extra fabric and sew this extra portion down. If confused, please refer to the pictures.
F. Sew MainF and TopF together leaving a 1/4 seam along the edge.
Step 3: Adding the Elastic Band
After sewing the two portions together, flip the hat. The folded flap should be on the outside now.
Cut about a 6 inch long piece of elastic band. Start with either the left or right side of the thick portion of the hat. About 4 inches from the edge, sew the elastic down on the inside of the flap. Sew down the flap to the fold and along the edge to the other side. Close up the gap by sewing down the other end of elastic 4 inches from the other side. After releasing the hat, it should scrunch together.
Note: If you feel the hat is still too loose, you can either shorten the length of the elastic or sew further out from the middle of the hat.
Step 4: Reaping the Compliments
Final outcome: One Awesome looking surgical/scrub cap.
Check out this video for more help – https://www.instructables.com/id/DIY-SurgicalScrub-Hat/
At AHA Press Briefing, Hospitals Describe Dire Need for More Federal Funding to Fight Pandemic and Care for Patients and Communities
At an AHA press briefing today, hospital and health system leaders from across the country described the urgent need for federal aid to ensure that frontline medical personnel have the tools and resources they need to effectively respond to the COVID-19 crisis.
“We’ve already seen facilities facing shortages of needed equipment and high expenses in providing critical care and this hurts our country’s ability to respond,” said AHA President and CEO Rick Pollack. “…The reality is that we are in a war in which hospitals and health systems are on the frontlines and our health care workers are putting their lives on the line to fight this battle … No one ever sends their troops into battle without the right protection and ammunition and tools.”
The AHA, American Medical Association and American Nurses Association Thursday urged congressional leaders to provide $100 billion to front line health care personnel and providers and direct federal agencies to infuse funds immediately so they can take the necessary steps to fight the pandemic.
Pollack also emphasized the need for having enough tests and getting the test results as quickly as possible in order to have a more accurate picture of the infection rate.
“Ensuring the safety of the patients, protecting health care workers and supporting the health and safety of our community is what we’re all about, and it requires every part of the health care sector to work together, from those on the front lines to the federal, state and local government,” Pollack said. “Equipped with the right tools, guidance and resources we will do our very best to protect lives and keep people healthy.”
Scott Graham, CEO of Three Rivers and North Valley Hospitals in rural Washington state said, “We’re trying to figure out how to stay in business.” Because of the mandates for social distancing and state’s cancellation of elective surgeries, he said “the revenue that typically comes in that we need to cover the cost of operating has dried up. …we are now in a negative cash position and are using credit. We will exhaust all avenues to make payroll in the next three or four weeks.”
Even before the COVID-19 crisis, One Brooklyn Health System in New York was relying on more than $20 million a month in support from New York State to keep its safety net hospitals open, said LaRay Brown, its president and CEO. “We had less than two weeks cash on hand before COVID-19,” she said. “We are now looking at an additional cost of $30-$34 million a month from projected staff increases to cover surge capacity” and replace staff who are on furlough, self-isolating or must care for their children while city schools are closed.
Kevin Donovan, president and CEO of LRGHealthcare in central New Hampshire, projects his health system’s freeze on elective services during the public health crisis will cost at least $50 million. “Prior to this crisis, much like my colleagues, we were in extremely poor financial condition,” he said, with “only a handful of cash on hand” and no debt capacity to borrow money.
“I think these stories are reflective of the experiences of thousands of hospitals across the country,” Pollack said. “That’s why the legislation being considered on the Hill right now is so important in terms of providing needed support.”
LRGH COVID-19 Hotline
During normal business hours we encourage you to contact your Primary Care Provider (PCP) or the Hotline.
The LRGH Covid-19 hotline (603-527-7069) is available for patients to call DAILY 7am-5pm to answer your questions. It is staffed with a nurse who can help triage symptoms you may be experiencing and provide you guidance for further follow up. You can also visit our website at www.concordhospital-laconia.org for up to date information.
After normal business hours If you are concerned that you may have Covid-19 symptoms, please call the State Public Health Department at 603-271-4496. If you are experiencing a medical emergency, please call 911 or go to your nearest emergency department.
We Can All Do Something to Help
The COVID-19 pandemic is scary, and it’s natural to feel overwhelmed by what is going on. Unfortunately, the reality is that things will get a lot worse in the coming weeks and months, and many people in our communities are going to need help. The good news is that there are things you can do today to change the course of the pandemic and help our community get through it.
1. Social Distancing: This is by far the most important thing you can do to help our community, not to mention to protect yourself and your family. Please share these resources with anyone you know who is skeptical about having to stay home.
Why outbreaks of coronavirus spread exponentially, and how to “flatten the curve” –Washington Post
Social Distancing: This is not a snow day – Medium.com
COVID-19 is different from flu, and we must respond differently – CNN
2. Food Supports: Donate to a Got Lunch organization in your town and to your local food pantry.
Yesterday, the Governor announced that schools are closed, but that they will distribute food to families whose children participate in their school’s food programs. We know that local Got Lunch! organizations have been mobilizing to distribute groceries to families during this crisis. Both will be a big help to families who are losing income due to the pandemic.
Food pantries will help elderly or disabled residents of low-income and families who don’t have a Got Lunch program in their town.
You can also offer to go get groceries for your relatives and neighbors who are over the age of 60 or have underlying health problems. These people should be self-isolating at home – it is dangerous for them to go anywhere.
3. Support Local Businesses: You can stay home while still spending money at your favorite local businesses by buying gift certificates to use later. The vast majority of businesses in our region and state are small and locally owned and they will be hit hard by this crisis. The more we support them, the more they can support their employees during this difficult time.
The days ahead will be challenging. But we are not helpless in the face of this pandemic. Each of us has the power change the course of history with our choices over the coming weeks and months. There is a strong spirit of generosity and community here in the Lakes Region – we have a lot of practice giving back and helping out! So I know that, while we may all experience sadness in the days to come, we will also feel moments of great hope as we work together to overcome this unprecedented challenge.
Yours in hope and community,
Carmen R. Lorentz
Visitation Policy/Message COVID 19
Message to our community
Out of an abundance of caution, LRGHealthcare will restrict all visitors to Franklin Regional Hospital, Lakes Region General Hospital, and all affiliates of LRGHealthcare, effective Noon, Sunday, March 15, 2020.
We are taking this measure to protect our patients and employees from potential exposure to Coronavirus (COVID-19).
In addition to this temporary visitation policy, we are suspending all community meetings held on premises, community education classes and community access to our cafeterias.
If you have a loved one who is critically ill and it is imperative that you see them, please call 603-524-3211 to contact a hospital leadership representative on call. Requests will be reviewed on a case by case basis.
PLEASE NOTE: During this restricted visitation time, if you want to have patients receive a delivery of flowers, our staff will ensure that they receive them.
Thank you for your continued commitment to keep our community healthy.
The New Hampshire Department of Health and Human Services has developed a website just for COVID-19 information.
State Launches 2-1-1 COVID-19 Hotline
CONCORD, NH – Today, Governor Chris Sununu, the New Hampshire Department of Health and Human Services, and NH Homeland Security and Emergency Management, announced that 211NH has been mobilized to handle all COVID-19 related calls from New Hampshire residents. All residents with questions or concerns surrounding the COVID-19 outbreak can call 2-1-1.
“211NH will serve as a coordinated and streamlined process for any Granite Stater concerned about the coronavirus,” said Governor Chris Sununu. “Now that it is up and running, any New Hampshire residents can call with questions or concerns. I would like to thank the folks at Granite United Way and Public Health for working around the clock to stay on top of this evolving public health situation by making this critical resource available 24/7.”
“It is important during an outbreak that residents get the information they need to protect their health and the health of their community,” said HHS Commissioner Lori Shibinette. “2-1-1 provides that resource for our residents to get the most up to date and accurate information about the presence of coronavirus in New Hampshire.”
211NH is New Hampshire’s statewide, comprehensive, information and referral service operated by Granite United Way and will replace the current Department of Public Health Hotline (603-271-4496) for COVID-19 related questions.
Members of the media and local city and town officials, as well as emergency management officials should still call the state’s Joint Information Center.
LRGH COVID-19 Hotline
During normal business hours we encourage you to contact your Primary Care Provider (PCP) or the Hotline.
The Covid-19 hotline (603-527-7069) is available for patients to call Monday-Friday 8am-4pm to answer your questions. It is staffed with a nurse who can help triage symptoms you may be experiencing and provide you guidance for further follow up. You can also visit our website at www.concordhospital-laconia.org for up to date information.
After normal business hours If you are concerned that you may have Covid-19 symptoms, please call the State Public Health Department at 603-271-4496. If you are experiencing a medical emergency, please call 911 or go to your nearest emergency department.
Thank you!
Fact sheet:
Coronavirus disease 2019 (COVID-19)
What it is
Coronavirus disease 2019 (COVID-19) is a respiratory illness which was first identified in Wuhan, Hubei Province, China.
How it spreads
The CoVID-19 virus is spread from person-to-person, although the CDC does not yet know how easily it is spread between people.
The scope of the problem
- COVID-19 has spread to other countries, with significant outbreaks in South Korea and sustained cases of community transmission in Iran, Italy and Japan, according to the CDC.
- There are more than 81,000 confirmed cases worldwide and more than 3200 deaths.
- There have been 60 confirmed cases in the United States (see https://www.cdc.gov/coronavirus/2019-ncov/cases-in-us.html for the most updated case count).
- As of March 4th, two patients in NH have tested (presumptive) positive for COVID-19 and others are undergoing testing.
How LRGHealthcare is Prepared
- With guidance from the NH DHHS, we have plans in place to manage patients with COVID-19 while safeguarding patients, hospital visitors, health care workers and the community at large.
- Travel screenings are in place for all intake staff to identify higher risk patients.
- If a patient tests positive for the illness, the appropriate protocol is already in place, including isolation of the patient in an Airborne Isolation room.
What the Public Should Do
- Because it is currently the cold and flu season, the CDC recommends getting the flu vaccine if you have not already. Influenza symptoms can mimic COVID-19 symptoms.
- Individuals should continue to exercise standard safety measures, including not touching your eyes, nose and mouth with unwashed hands.
- Wash your hands often with soap and water for at least 20 seconds, especially after using the bathroom; use an alcohol-based hand sanitizer if soap and water are not available. (In most circumstances, alcohol-based hand sanitizers are highly effective alternatives to soap and water for health care providers in the workplace.)
- Do not go to work if you are sick and do not send your children to school if they are sick.
- If you are sick and have traveled to a region where COVID-19 is spreading, or have been in contact with someone suspected of having COVID-19, call your health care provider immediately for recommendations on how best to be evaluated; do not go to a hospital, urgent care site, or outpatient clinic without calling ahead to report your travel history.
The Symptoms
The main symptoms of the illness include fever, dry cough, shortness of breath and myalgia. The symptoms may appear in as few as two days or as many as two weeks after exposure.
Severity of the illness
COVID-19 can cause severe illness in some people, including death, although, based on preliminary information, the World Health Organization has stated that a large majority (82%) of COVID-19 cases have been mild; approximately 3% have been critical.
Treatment and Prevention
- There is currently no vaccine available for COVID-19. Vaccine development is in progress.
- There is currently no specific antiviral treatment recommended for COVID-19. Research studies assessing potential treatments are in progress.
Current CDC Travel Warnings
- The CDC has issued travel warnings to U.S. residents, recommending that all travelers avoid all nonessential travel to China, Iran, Italy and South Korea.
- Additionally, the CDC is advising that older adults and those with chronic medical conditions consider postponing nonessential travel to Japan, as that country is experiencing sustained community spread of COVID-19.
- Before traveling to any country, the CDC advises that you visit cdc.gov/coronavirus/2019-ncov/travelers/index.html to see the current risks and advisories.
Current LRGHealthcare Travel Advisory
- LRGHealthcare strongly discourages employees from traveling to any CDC Warning level 3 and Alert level 2 country. This is a rapidly evolving situation; additional countries may be added to the CDC travel advisory list as circumstances change.
For Additional Information
- LRGHealthcare actively monitoring COVID-19 and has a helpful website for faculty and students.
- Visit the CDC website for updates on COVID-19 including current travel warnings and alerts.
The New Hampshire Department of Health and Human Services (DHHS) and the Division of Public Health Services (DPHS) announced the first presumptive positive test result in New Hampshire for COVID-19, the disease caused by the new coronavirus today.
State Epidemiologist Dr. Benjamin Chan said, “This positive test is in an individual who traveled to Italy and developed symptoms consistent with COVID-19 within several days of travel. At this time, there is no evidence of more widespread community transmission in New Hampshire.”
The NH Public Health Laboratories (PHL) conducted the test and identified the presumptive positive result. The patient’s specimen is being sent to the Center for Disease Control (CDC) for confirmatory testing. The CDC is conducting confirmatory tests on all state laboratory tests that are found to be presumptively positive for COVID-19.
Because COVID-19, and all respiratory illnesses, are most commonly spread through respiratory droplets, residents should take the same precautions as those recommended to prevent the spread of influenza:
- Stay home and avoid public places when sick (i.e., social distancing)
- Cover mouth and nose when coughing and sneezing
- Wash hands frequently
- Avoid being within 6 feet (close contact) of a person who is sick
- Avoid sharing drinks, smoking/vaping devices, or other utensils or objects that may transmit saliva
- Disinfect frequently touched surfaces
We have convened a multi-disciplinary, Executive Steering Committee to assess the COVID-19 (Coronavirus) situation and determine our course of action moving forward.
LRGHealthcare is committed to keeping our community safe and apprised of the COVID-19 (Coronavirus) situation.